Hair Loss Is Another Consequence of the Pandemic
Annrene Rowe, a 67 year old Florida woman was getting ready to celebrate her 10th wedding anniversary this summer when she noticed a bald spot on her scalp. Soon, her once thick and shoulder-length hair started falling out in clumps. “I was crying hysterically,” said Rowe.
Rowe was hospitalized for 12 days in April with symptoms of the coronavirus. She found very similar stories in online COVID-19 survivor groups. Many said that several months after contracting the virus, they began shedding large amounts of hair.
Doctors say they are also seeing many more patients with hair loss. They believe this phenomenon is related to the coronavirus pandemic, affecting both people who actually had the virus, as well as those who never even became sick. In normal times, some people shed noticeable amounts of hair after a stressful experience, such as an illness, major surgery, or emotional trauma.
Many patients recovering from COVID-19 are experiencing hair loss not from the virus itself, but from the stress of fighting it off. People who never even contracted the virus are also losing hair due to emotional stress from job loss, financial strain, deaths of family members, or other devastating consequences of the pandemic.
In a July survey about post-COVID-19 symptoms among 1,567 members of a survivors’ group, 423 people reported unusual hair loss, according to the group, Survivor Corps, and Natalie Lambert, an associate research professor at Indiana University School of Medicine that helped conduct the survey.
Dr. Emma Guttman-Yassky, the incoming chair of the dermatology department at Mount Sinai’s Icahn School of Medicine, said she has treated many front-line medical workers for hair loss, including her hospital’s employees. “Some of them had COVID, but not all of them,” she said. “It’s the stress of the situation. They were apart from their families. They worked for many hours.”
Doctors say the condition should be temporary for most patients, but it could last months.
There are two types of hair loss the pandemic seems to be triggering.
In one condition, called telogen effluvium, people shed much more than the typical 50 to 100 hairs per day. It usually begins several months after a stressful experience. It essentially involves a “tripping of the hair growth system,” said Dr. Sara Hogan, a dermatologist at the David Geffen School of Medicine at the University of California, Los Angeles, who has been seeing up to seven patients a day with the condition.
In healthy hair cycles, most hairs are in a growing phase, with a small percentage in a short resting phase, and only about 10% of hairs in a shedding or telogen phase. But with telogen effluvium, “people are shedding more, growing less,” Khetarpal said, and up to 50% of hair might skip ahead to the shedding phase, with only about 40% in the growth phase.The phenomenon, which some women also experience after pregnancy, typically lasts about six months. However, if stressful situations continue, some people develop a chronic shedding condition, Hogan said.
The other hair loss condition that is increasing now is alopecia areata, where the immune system attacks hair follicles. It usually starts with a patch of hair on the scalp or beard, said Dr. Mohammad Jafferany, a psychiatrist and dermatologist at Central Michigan University. “It is known to be associated with or exacerbated by psychological stress,” Jafferany said. Guttman-Yassky said that she has seen “a huge increase in this type of alopecia.”
Not all of the patients had COVID-19, she said, but the ones who did tended to progress very quickly from one or two bald patches to “losing hair all over the body,” including eyebrows and eyelashes. She said that might be because the storm of inflammation that some COVID patients experience elevates immune molecules linked to conditions like alopecia.
Experts don’t know exactly why stress triggers these conditions, which affect both women and men. It might be related to increased levels of cortisol, a stress hormone, or to effects on blood supply, Hogan said.
The hair loss itself can cause more stress, Khetarpal said, especially for women whose hair is often more closely tied to identity and self-confidence.
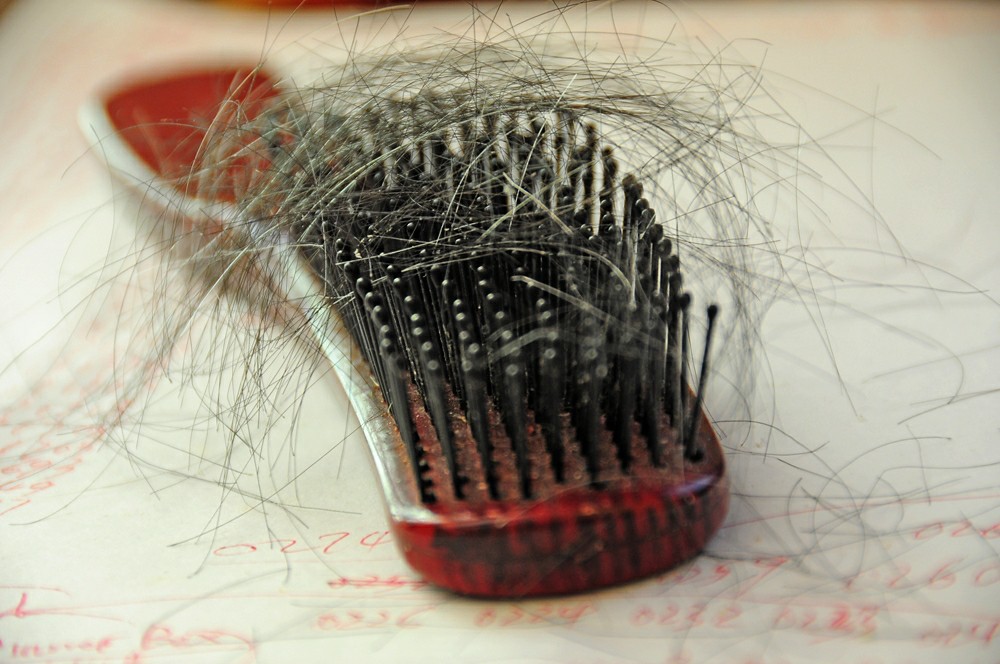
“It’s your trademark,” said Mary Lou Ostling, 77, a retired educator who lives in the Stuyvesant Town neighborhood of Manhattan. She was hospitalized for COVID-19 for eight days in the early spring and later noticed that “my hair started coming out in chunks,. She said, “I always was clearing hair out of the comb, brush, the sink.” Ostling said she also could tell that her hair wasn’t growing much because she wasn’t seeing roots that contrasted with the color she had previously dyed it. “I’ve always had very long, very thick, very curly hair,” she said. But in July, she had to cut it, saying “I couldn’t deal with it anymore.” When she came home from the hairdresser, she said, “my husband was just staring at me. He said, ‘I think I have a different wife.’ It was very depressing.” She said she has finally begun to notice some hair growth.
What You Should Do According to the Experts
Experts recommend good nutrition, vitamins such as biotin, and stress-reduction techniques like yoga, scalp massage, or mindfulness meditation. Some also recommend minoxidil, a hair growth drug, but Hogan warns patients that it can initially cause more hair loss before it starts working.
Guttman-Yassky said with alopecia areata, some cases resolve without treatment, and steroid injections can help some cases. Unfortunately, some can become permanent, especially if not treated early.
For people depressed or traumatized by hair loss, Jafferany recommends psychotherapy, but not necessarily medication as some antidepressants and anti-anxiety medications can increase hair loss.
When Liz Weidhorn, 44, of Fair Lawn, New Jersey, who tested positive for COVID-19 in March, noticed members of an online COVID group bemoaning hair loss, she told herself that if it happened to her, “I will take it with grace, and I’ll get a kick-ass hat.” But recently after showering, “I looked at my wet hair, and I could see so much scalp,” she said, “and I couldn’t believe how emotional I got.” She cried and called her husband in to look at it. “It’s really shocking,” she said. “It got me very sad.” Weidhorn, who writes a blog about baking pastry, started taking biotin, had her mother cut her hair, and is considering getting a headband.
Rowe, who managed the front desk for a wellness spa, has gone further. “I tried putting my hair in one of those messy buns, but it looks terrible with the bald spots on the sides,” she said. So she got wigs: “a really short pixie one, a pageboy one, a long curly one and a strawberry blonde one,” she said. “I’m trying to make the best of it.” Hogan said some patients find the situation so upsetting they avoided washing or brushing their hair altogether because they noticed the hair loss more during those activities. She tells them they shouldn’t be afraid of normal grooming.
She added, “Patients don’t like this when I say this, but they come around to it: Hair is not crucial for your survival.”







Recent Comments